Normal and Abnormal Blood Oxygen Levels During Sleep
Scientific Proofs - Oxygen Levels Decreases During Apneas. Even the most recent studies (2012) demonstrates the link between sleep apnea and oxygen desaturation. That's why the oximeter is an important tool in clinical assessment. With a finger pulse oximeter you can monitor yourself to see how effective is CPAP (you'll learn how to do this bellow). Normal oxygen saturation levels depend on altitude. The normal saturation at sea level is 96 to 98%. At 5,280 feet, it is 92 to 94%. So your reading of 96% by arterial blood gas (ABG) is normal. An ABG certainly measures oxygen saturation, but it does not measure lung function. Spirometry is a simple breathing test that measures lung function. Most people with copd, have a higher oxygen level when sitting. Why is mine 95-96 when sitting an gets up to 97-98 when active. Theirs gets lower. 2 doctor answers. 2 doctors weighed in. A 44-year-old male asked: Is a pulse oxygen level at 97 good? 96 oxygen level. A 46-year-old female asked: is 96 to 98% oxygen levels good i've stopped smoking 10 weeks now is this ok or signs of lung damage and copd? Timothy Wu answered. 18 years experience Vascular Surgery. Normal.: Anything around 95% or above is normal. 92% can be acceptable for certain disease states, such as copd. For neonates and young infants, the normal oxygen saturation level should range between 93% to 100%. For adults less than 70 years of age, the normal oxygen saturation level should range between 96% to 98%. For adults aged 70 and above, the normal oxygen saturation level should be greater than 94%.
Low sleep apnea oxygen level is a sign that your treatment for sleep apnea is not effective.
Patients with breathing problems during sleep (sleep apnea, COPD) often have low oxygen levels in their blood.
Keep in mind that anything below 90% oxygen level is dangerous to your body and require intervention. Another thing to consider is that the brain can only survive 4 minutes once oxygen is completely cut off.
In this page you'll learn:
- What should your oxygen level be during sleep,
- How sleep apnea affects the oxygen levels in your blood,
- How oxygen levels affect your body,
- The link between pregnancy and low oxygen levels in obese women,
- How to monitor oxygen saturation levels,
- What is the best finger oximeter to monitor blood oxygen levels,
- How to treat sleep apnea oxygen level.
Oxygen Levels During Sleep Apnea
In sleep, the upper airway muscle tone of the patients with sleep apnea tends to narrow and collapses temporarily. When this happens, the breathing stops accompanied by a drop in blood oxygen levels and arousal from sleep.
The low oxygen levels during sleep can make you feel very tired in the morning and will contribute to more restless sleep.
Boxshot ultimate free. Furthermore, when the oxygen levels start to drop, the carbon dioxide levels build up in your blood. Comracecomputers driver download for windows. This can lead to morning headaches, fatigue and sleepiness during the day.
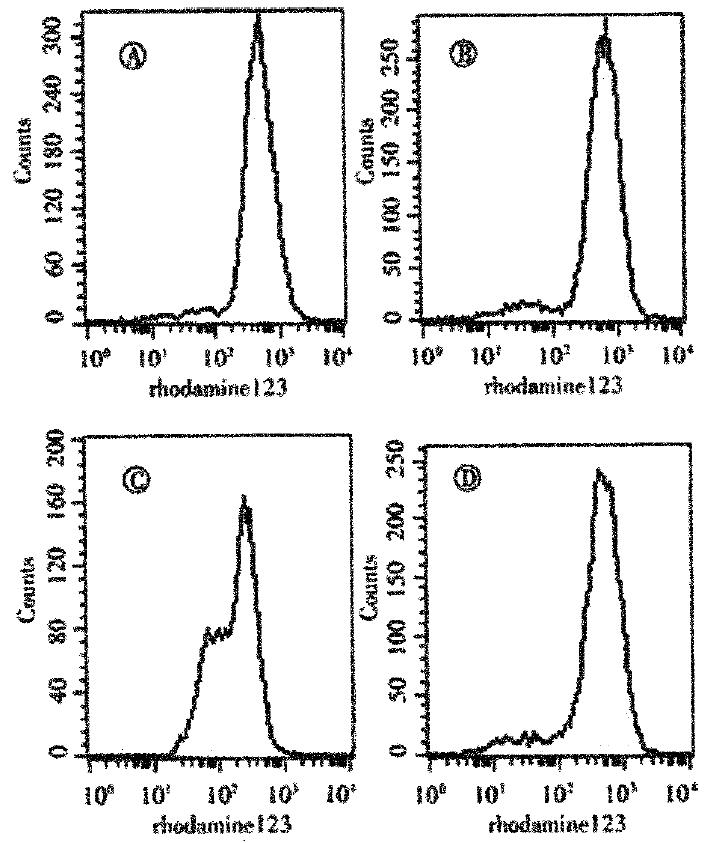
Scientific Proofs - Oxygen Levels Decreases During Apneas
Even the most recent studies (2012) demonstrates the link between sleep apnea and oxygen desaturation. That's why the oximeter is an important tool in clinical assessment.
With a finger pulse oximeter you can monitor yourself to see how effective is CPAP (you'll learn how to do this bellow). The device can also be used to diagnose sleep apnea, but only if you use a quality product.
For more information on how to use an oximeter to diagnose sleep apnea, read the portable pulse oximeter article.
How Does Sleep Apnea Oxygen Level Affect the Body?
Any value of blood oxygen level bellow 92% is abnormal. However, the number of desaturations and the time spent with abnormal oxygen levels is important.
Is 96 Oxygen Level Good
For example, if you only desaturated below 92% once or twice during a 7 hour sleep, and the desaturation level lasted only a couple of seconds, it's not a reason for worry.
Your body will be seriously affected when you'll have long term low oxygen levels. This can lead to:
- heart rhythm problems,
- increasing pressure on the right side of the heart,
- fluid build up in the body,
- heart failure,
- stroke.
Increasing the pressure on the right side of the heart
The right side of the heart has the role of pumping blood through the lungs, which requires a much lower pressure.
A higher pressure can lead to severe fluid buildup in the body that can cause life-threatening shortness of breath, heart failure and even death.
Please call your doctor urgently if you experience chest pain or shortness of breath that is not relieved by rest.
Monitoring Your Blood Oxygen Levels
If your doctor discovers that your blood oxygen level (oxygen saturation) is less than about 90% during the day (when you are resting), then your oxygen levels are probably dropping during the night. This means that you have sleep apnea, or other respiratory disorders, like UARS.
Your doctor may recommend overnight monitoring of your oxygen levels using am oximeter. In a sleep study, you usually have the oximeter attached on the finger.
You can use a portable oxygen saturation monitor or oximeter, a cool little device that can record your sleep apnea oxygen level and pulse rate during sleep. A medical approved oximeter is truly a great tool to see how well CPAP is working for you.
A tip before buying an oximeter: you would do well to invest in a recording oximeter with software. You can upload your data in a computer, and you can go to your sleep specialist with the results.
See an example in the followingvideo:
For more info about sleep study for sleep apnea, see sleep studies.
So, if you have a low blood oxygen level, follow up with the sleep study as soon as possible.
Continued drops in O2 levels will cause damage to cognitive function, short term memory, stroke and heart attack in your sleep, and a host of other problems.
Oxygen Levels in Pregnant Women
Overweight women who are pregnant or women who gain too much weight during pregnancy are at a higher risk of developing sleep apnea. This can cause a drop in blodd oxygen levels during sleep which can create complications for the baby.
So if you are overweight or gained a lot of weight during pregnancy, speak with your doctor to investigate if you have sleep apnea.
For more info about obesity, see sleep apnea and obesity.
Improving Sleep Apnea Oxygen Level
Patients with sleep apnea are usually treated with CPAP machines. If apnea episodes disappear, the oxygen levels will improve to normal levels.
How often should you use the CPAP?
If your doctor prescribed CPAP therapy, you should NEVER go a night EVER without a CPAP on or even take a nap without one.
More strategies to treat sleep apnea:
If your oxygen saturations drop significantly and persist during the night, you may benefit from overnight oxygen delivered by nasal masks or nasal prongs.
CPAP and Oxygen Levels During Sleep
You can have low oxygen levels during sleep even if you use the CPAP. This means that your CPAP doesn't have the desired effect.
That's why is important to monitor your oxygen and pulse rate.
To keep a better eye on your sleep apnea oxygen level you might consider purchasing a finger pulse oximeter.
Remember: don't use inferior equipment to measure your well-being and don't change anything without checking that information with a second opinion or proper equipment.
Sleep Apnea › Sleep Apnea Side Effects › Sleep Apnea Oxygen Level
Last Updated: December 17, 2020
The COVID-19 Treatment Guidelines Panel’s (the Panel’s) recommendations below emphasize recommendations from the Surviving Sepsis Campaign Guidelines for adult sepsis, pediatric sepsis, and COVID-19.
Nonmechanically Ventilated Adults With Hypoxemic Respiratory Failure
Recommendations
- For adults with COVID-19 and acute hypoxemic respiratory failure despite conventional oxygen therapy, the Panel recommends high-flow nasal cannula (HFNC) oxygen over noninvasive positive pressure ventilation (NIPPV) (BIIa).
- In the absence of an indication for endotracheal intubation, the Panel recommends a closely monitored trial of NIPPV for adults with COVID-19 and acute hypoxemic respiratory failure and for whom HFNC is not available (BIIa).
- For patients with persistent hypoxemia despite increasing supplemental oxygen requirements in whom endotracheal intubation is not otherwise indicated, the Panel recommends considering a trial of awake prone positioning to improve oxygenation (CIIa).
- The Panel recommends against using awake prone positioning as a rescue therapy for refractory hypoxemia to avoid intubation in patients who otherwise meet the indications for intubation and mechanical ventilation (AIII).
- If intubation becomes necessary, the procedure should be performed by an experienced practitioner in a controlled setting due to the enhanced risk of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) exposure to health care practitioners during intubation (AIII).
Rationale
Severe illness in COVID-19 typically occurs approximately 1 week after the onset of symptoms. The most common symptom is dyspnea, which is often accompanied by hypoxemia. Patients with severe disease typically require supplemental oxygen and should be monitored closely for worsening respiratory status because some patients may progress to acute respiratory distress syndrome (ARDS).
Goal of Oxygenation
The optimal oxygen saturation (SpO2) in adults with COVID-19 is uncertain. However, a target SpO2 of 92% to 96% seems logical considering that indirect evidence from experience in patients without COVID-19 suggests that an SpO2 <92% or >96% may be harmful.
Regarding the potential harm of maintaining an SpO2 <92%, a trial randomly assigned ARDS patients without COVID-19 to either a conservative oxygen strategy (target SpO2 of 88% to 92%) or a liberal oxygen strategy (target SpO2 ≥96%). The trial was stopped early due to futility after enrolling 205 patients, but in the conservative oxygen group there was increased mortality at 90 days (between-group risk difference of 14%; 95% CI, 0.7% to 27%) and a trend toward increased mortality at 28-days (between-group risk difference of 8%; 95% CI, -5% to 21%).1
Regarding the potential harm of maintaining an SpO2 >96%, a meta-analysis of 25 randomized trials involving patients without COVID-19 found that a liberal oxygen strategy (median SpO2 of 96%) was associated with an increased risk of in-hospital mortality compared to a lower SpO2 comparator (relative risk 1.21; 95% CI, 1.03–1.43).2
Acute Hypoxemic Respiratory Failure
In adults with COVID-19 and acute hypoxemic respiratory failure, conventional oxygen therapy may be insufficient to meet the oxygen needs of the patient. Options for providing enhanced respiratory support include HFNC, NIPPV, intubation and invasive mechanical ventilation, or extracorporeal membrane oxygenation (ECMO).
High-Flow Nasal Cannula and Noninvasive Positive Pressure Ventilation
HFNC is preferred over NIPPV in patients with acute hypoxemic respiratory failure based on data from an unblinded clinical trial in patients without COVID-19 who had acute hypoxemic respiratory failure. Study participants were randomized to HFNC, conventional oxygen therapy, or NIPPV. The patients in the HFNC group had more ventilator-free days (24 days) than those in the conventional oxygen therapy group (22 days) or NIPPV group (19 days) (P = 0.02), and 90-day mortality was lower in the HFNC group than in either the conventional oxygen therapy group (HR 2.01; 95% CI, 1.01–3.99) or the NIPPV group (HR 2.50; 95% CI, 1.31–4.78).3 In the subgroup of more severely hypoxemic patients (PaO2/FiO2 mm Hg ≤200), the intubation rate was lower for HFNC than for conventional oxygen therapy or NIPPV (HR 2.07 and 2.57, respectively).
The trial’s findings were corroborated by a meta-analysis of eight trials with 1,084 patients conducted to assess the effectiveness of oxygenation strategies prior to intubation. Compared to NIPPV, HFNC reduced the rate of intubation (OR 0.48; 95% CI, 0.31–0.73) and ICU mortality (OR 0.36; 95% CI, 0.20–0.63).4
NIPPV may generate aerosol spread of SARS-CoV-2 and thus increase nosocomial transmission of the infection.5,6 It remains unclear whether HFNC results in a lower risk of nosocomial SARS-CoV-2 transmission than NIPPV.
Prone Positioning for Nonintubated Patients
Although prone positioning has been shown to improve oxygenation and outcomes in patients with moderate-to-severe ARDS who are receiving mechanical ventilation,7,8 there is less evidence regarding the benefit of prone positioning in awake patients who require supplemental oxygen without mechanical ventilation. In a case series of 50 patients with COVID-19 pneumonia who required supplemental oxygen upon presentation to a New York City emergency department, awake prone positioning improved the overall median oxygen saturation of the patients. However, 13 patients still required intubation due to respiratory failure within 24 hours of presentation to the emergency department.9 Other case series of patients with COVID-19 requiring oxygen or NIPPV have similarly reported that awake prone positioning is well-tolerated and improves oxygenation,10-12 with some series also reporting low intubation rates after proning.10,12
A prospective feasibility study of awake prone positioning in 56 patients with COVID-19 receiving HFNC or NIPPV in a single Italian hospital found that prone positioning for ≤3 hours was feasible in 84% of the patients. There was a significant improvement in oxygenation during prone positioning (PaO2/FiO2 181 mm Hg in supine position vs. PaO2/FiO2 286 mm Hg in prone position). However, when compared with baseline oxygenation before initiation of prone positioning, this improvement in oxygenation was not sustained (PaO2/FiO2 of 181 mm Hg and 192 mm Hg at baseline and 1 hour after resupination, respectively). Among patients put in the prone position, there was no difference in intubation rate between patients who maintained improved oxygenation (i.e., responders) and nonresponders.9
A prospective, multicenter observational cohort study in Spain and Andorra evaluated the effect of prone positioning on the rate of intubation in COVID-19 patients with acute respiratory failure receiving HFNC. Of the 199 patients requiring HFNC, 55 (27.6%) were treated with prone positioning. Although the time to intubation was 1 day (IQR 1.0–2.5) in patients receiving HFNC and prone positioning versus 2 days [IQR 1.0–3.0] in patients receiving only HFNC (P = 0.055), the use of awake prone positioning did not reduce the risk of intubation (RR 0.87; 95% CI, 0.53–1.43; P = 0.60).13
Overall, despite promising data, it is unclear which hypoxemic, nonintubated patients with COVID-19 pneumonia benefit from prone positioning, how long prone positioning should be continued, or whether the technique prevents the need for intubation or improves survival.10
Appropriate candidates for awake prone positioning are those who can adjust their position independently and tolerate lying prone. Awake prone positioning is contraindicated in patients who are in respiratory distress and who require immediate intubation. Awake prone positioning is also contraindicated in patients who are hemodynamically unstable, patients who recently had abdominal surgery, and patients who have an unstable spine.14 Awake prone positioning is acceptable and feasible for pregnant patients and can be performed in the left lateral decubitus position or the fully prone position.15
Intubation for Invasive Mechanical Ventilation
It is essential to monitor hypoxemic patients with COVID-19 closely for signs of respiratory decompensation. To ensure the safety of both patients and health care workers, intubation should be performed in a controlled setting by an experienced practitioner.
Mechanically Ventilated Adults
Recommendations
For mechanically ventilated adults with COVID-19 and ARDS:
- The Panel recommends using low tidal volume (VT) ventilation (VT 4–8 mL/kg of predicted body weight) over higher VT ventilation (VT >8 mL/kg) (AI).
- The Panel recommends targeting plateau pressures of <30 cm H2O (AIIa).
- The Panel recommends using a conservative fluid strategy over a liberal fluid strategy (BIIa).
- The Panel recommends against the routine use of inhaled nitric oxide (AIIa).
Rationale
96 Oxygen Level Child
There is no evidence that ventilator management of patients with hypoxemic respiratory failure due to COVID-19 should differ from ventilator management of patients with hypoxemic respiratory failure due to other causes.
Positive End-Expiratory Pressure and Prone Positioning in Mechanically Ventilated Adults With Moderate to Severe Acute Respiratory Distress Syndrome
Recommendations
For mechanically ventilated adults with COVID-19 and moderate-to-severe ARDS:
- The Panel recommends using a higher positive end-expiratory pressure (PEEP) strategy over a lower PEEP strategy (BIIa).
- For mechanically ventilated adults with COVID-19 and refractory hypoxemia despite optimized ventilation, the Panel recommends prone ventilation for 12 to 16 hours per day over no prone ventilation (BIIa).
Rationale
PEEP is beneficial in patients with ARDS because it prevents alveolar collapse, improves oxygenation, and minimizes atelectotrauma, a source of ventilator-induced lung injury. A meta-analysis of individual patient data from the three largest trials that compared lower and higher levels of PEEP in patients without COVID-19 found lower rates of ICU mortality and in-hospital mortality with higher PEEP in those with moderate (PaO2/FiO2 100–200 mm Hg) and severe ARDS (PaO2/FiO2 <100 mm Hg).16
Although there is no clear standard as to what constitutes a high level of PEEP, one conventional threshold is >10 cm H2O.17 Recent reports have suggested that, in contrast to patients with non-COVID-19 causes of ARDS, some patients with moderate or severe ARDS due to COVID-19 have normal static lung compliance and thus, in these patients, higher PEEP levels may cause harm by compromising hemodynamics and cardiovascular performance.18,19 Other studies reported that patients with moderate to severe ARDS due to COVID-19 had low compliance, similar to the lung compliance seen in patients with conventional ARDS.20-23 These seemingly contradictory observations suggest that COVID-19 patients with ARDS are a heterogeneous population and assessment for responsiveness to higher PEEP should be individualized based on oxygenation and lung compliance. Clinicians should monitor patients for known side effects of higher PEEP, such as barotrauma and hypotension.
Neuromuscular Blockade in Mechanically Ventilated Adults With Moderate to Severe Acute Respiratory Distress Syndrome
Recommendations
For mechanically ventilated adults with COVID-19 and moderate-to-severe ARDS:
- The Panel recommends using, as needed, intermittent boluses of neuromuscular blocking agents (NMBA) or continuous NMBA infusion to facilitate protective lung ventilation (BIIa).
- In the event of persistent patient-ventilator dyssynchrony, or in cases where a patient requires ongoing deep sedation, prone ventilation, or persistently high plateau pressures, the Panel recommends using a continuous NMBA infusion for up to 48 hours as long as patient anxiety and pain can be adequately monitored and controlled (BIII).
Rationale
The recommendation for intermittent boluses of NMBA or continuous infusion of NMBA to facilitate lung protection may require a health care provider to enter the patient’s room frequently for close clinical monitoring. Therefore, in some situations, the risks of SARS-CoV-2 exposure and the need to use personal protective equipment for each entry into a patient’s room may outweigh the benefit of NMBA treatment.
Rescue Therapies for Mechanically Ventilated Adults With Acute Respiratory Distress Syndrome
Recommendations
For mechanically ventilated adults with COVID-19, severe ARDS, and hypoxemia despite optimized ventilation and other rescue strategies:
- The Panel recommends using recruitment maneuvers rather than not using recruitment maneuvers (CIIa).
- If recruitment maneuvers are used, the Panel recommends against using staircase (incremental PEEP) recruitment maneuvers (AIIa).
- The Panel recommends using an inhaled pulmonary vasodilator as a rescue therapy; if no rapid improvement in oxygenation is observed, the treatment should be tapered off (CIII).
Rationale
There are no studies to date assessing the effect of recruitment maneuvers on oxygenation in severe ARDS due to COVID-19. However, a systematic review and meta-analysis of six trials of recruitment maneuvers in non-COVID-19 patients with ARDS found that recruitment maneuvers reduced mortality, improved oxygenation 24 hours after the maneuver, and decreased the need for rescue therapy.24 Because recruitment maneuvers can cause barotrauma or hypotension, patients should be closely monitored during recruitment maneuvers. If a patient decompensates during recruitment maneuvers, the maneuver should be stopped immediately. The importance of properly performing recruitment maneuvers was illustrated by an analysis of eight randomized controlled trials in non-COVID-19 patients (n = 2,544) which found that recruitment maneuvers did not reduce hospital mortality (RR 0.90; 95% CI, 0.78–1.04). Subgroup analysis found that traditional recruitment maneuvers significantly reduced hospital mortality (RR 0.85; 95% CI, 0.75–0.97), whereas incremental PEEP titration recruitment maneuvers increased mortality (RR 1.06; 95% CI, 0.97–1.17).25
Although there are no published studies of inhaled nitric oxide in patients with COVID-19, a Cochrane review of 13 trials of inhaled nitric oxide use in patients with ARDS found no mortality benefit.26 Because the review showed a transient benefit in oxygenation, it is reasonable to attempt inhaled nitric oxide as a rescue therapy in COVID patients with severe ARDS after other options have failed. However, if there is no benefit in oxygenation with inhaled nitric oxide, it should be tapered quickly to avoid rebound pulmonary vasoconstriction that may occur with discontinuation after prolonged use.
96% Oxygen Level
References
96 Oxygen Level Covid
- Barrot L, Asfar P, Mauny F, et al. Liberal or conservative oxygen therapy for acute respiratory distress syndrome. N Engl J Med. 2020;382(11):999-1008. Available at: https://www.ncbi.nlm.nih.gov/pubmed/32160661.
- Chu DK, Kim LH, Young PJ, et al. Mortality and morbidity in acutely ill adults treated with liberal versus conservative oxygen therapy (IOTA): a systematic review and meta-analysis. Lancet. 2018;391(10131):1693-1705. Available at: https://www.ncbi.nlm.nih.gov/pubmed/29726345.
- Frat JP, Thille AW, Mercat A, et al. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med. 2015;372(23):2185-2196. Available at: https://www.ncbi.nlm.nih.gov/pubmed/25981908.
- Ni YN, Luo J, Yu H, Liu D, Liang BM, Liang ZA. The effect of high-flow nasal cannula in reducing the mortality and the rate of endotracheal intubation when used before mechanical ventilation compared with conventional oxygen therapy and noninvasive positive pressure ventilation. A systematic review and meta-analysis. Am J Emerg Med. 2018;36(2):226-233. Available at: https://www.ncbi.nlm.nih.gov/pubmed/28780231.
- Tran K, Cimon K, Severn M, Pessoa-Silva CL, Conly J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS One. 2012;7(4):e35797. Available at: https://www.ncbi.nlm.nih.gov/pubmed/22563403.
- Yu IT, Xie ZH, Tsoi KK, et al. Why did outbreaks of severe acute respiratory syndrome occur in some hospital wards but not in others? Clin Infect Dis. 2007;44(8):1017-1025. Available at: https://www.ncbi.nlm.nih.gov/pubmed/17366443.
- Guerin C, Reignier J, Richard JC, et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368(23):2159-2168. Available at: https://www.ncbi.nlm.nih.gov/pubmed/23688302.
- Fan E, Del Sorbo L, Goligher EC, et al. An official American Thoracic Society/European Society of Intensive Care Medicine/Society of Critical Care Medicine Clinical Practice guideline: mechanical ventilation in adult patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2017;195(9):1253-1263. Available at: https://www.ncbi.nlm.nih.gov/pubmed/28459336.
- Caputo ND, Strayer RJ, Levitan R. Early self-proning in awake, non-intubated patients in the emergency department: a single ED's experience during the COVID-19 pandemic. Acad Emerg Med. 2020;27(5):375-378. Available at: https://www.ncbi.nlm.nih.gov/pubmed/32320506.
- Sun Q, Qiu H, Huang M, Yang Y. Lower mortality of COVID-19 by early recognition and intervention: experience from Jiangsu Province. Ann Intensive Care. 2020;10(1):33. Available at: https://www.ncbi.nlm.nih.gov/pubmed/32189136.
- Elharrar X, Trigui Y, Dols AM, et al. Use of prone positioning in nonintubated patients With COVID-19 and hypoxemic acute respiratory failure. JAMA. 2020;323(22):2336-2338. Available at: https://www.ncbi.nlm.nih.gov/pubmed/32412581.
- Sartini C, Tresoldi M, Scarpellini P, et al. Respiratory parameters in patients with COVID-19 after using noninvasive ventilation in the prone position outside the intensive care unit. JAMA. 2020;323(22):2338-2340. Available at: https://www.ncbi.nlm.nih.gov/pubmed/32412606.
- Ferrando C, Mellado-Artigas R, Gea A, et al. Awake prone positioning does not reduce the risk of intubation in COVID-19 treated with high-flow nasal oxygen therapy: a multicenter, adjusted cohort study. Crit Care. 2020;24(1):597. Available at: https://www.ncbi.nlm.nih.gov/pubmed/33023669.
- Bamford P, Bentley A, Dean J, Whitmore D, Wilson-Baig N. ICS guidance for prone positioning of the conscious COVID patient. Intensive Care Society. 2020. Available at: https://emcrit.org/wp-content/uploads/2020/04/2020-04-12-Guidance-for-conscious-proning.pdf. Accessed December 8, 2020.
- Society for Maternal Fetal Medicine. Management considerations for pregnant patients with COVID-19. 2020. Available at: https://s3.amazonaws.com/cdn.smfm.org/media/2336/SMFM_COVID_Management_of_COVID_pos_preg_patients_4-30-20_final.pdf. Accessed December 8, 2020.
- Briel M, Meade M, Mercat A, et al. Higher vs. lower positive end-expiratory pressure in patients with acute lung injury and acute respiratory distress syndrome: systematic review and meta-analysis. JAMA. 2010;303(9):865-873. Available at: https://www.ncbi.nlm.nih.gov/pubmed/20197533.
- Alhazzani W, Moller MH, Arabi YM, et al. Surviving Sepsis Campaign: guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID-19). Crit Care Med. 2020;48(6):e440-e469. Available at: https://www.ncbi.nlm.nih.gov/pubmed/32224769.
- Marini JJ, Gattinoni L. Management of COVID-19 respiratory distress. JAMA. 2020;323(22):2329-2330. Available at: https://www.ncbi.nlm.nih.gov/pubmed/32329799.
- Tsolaki V, Siempos I, Magira E, Kokkoris S, Zakynthinos GE, Zakynthinos S. PEEP levels in COVID-19 pneumonia. Crit Care. 2020;24(1):303. Available at: https://www.ncbi.nlm.nih.gov/pubmed/32505186.
- Bhatraju PK, Ghassemieh BJ, Nichols M, et al. COVID-19 in critically ill patients in the Seattle region - case series. N Engl J Med. 2020;382(21):2012-2022. Available at: https://www.ncbi.nlm.nih.gov/pubmed/32227758.
- Cummings MJ, Baldwin MR, Abrams D, et al. Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: a prospective cohort study. Lancet. 2020;395(10239):1763-1770. Available at: https://www.ncbi.nlm.nih.gov/pubmed/32442528.
- Ziehr DR, Alladina J, Petri CR, et al. Respiratory pathophysiology of mechanically ventilated patients with COVID-19: a cohort study. Am JRespir Crit Care Med. 2020;201(12):1560-1564. Available at: https://www.ncbi.nlm.nih.gov/pubmed/32348678.
- Schenck EJ, Hoffman K, Goyal P, et al. Respiratory mechanics and gas exchange in COVID-19 associated respiratory failure. Ann Am Thorac Soc. 2020;17(9):1158-1161. Available at: https://www.ncbi.nlm.nih.gov/pubmed/32432896.
- Goligher EC, Hodgson CL, Adhikari NKJ, et al. Lung recruitment maneuvers for adult patients with acute respiratory distress syndrome. a systematic review and meta-analysis. Ann Am Thorac Soc. 2017;14(Supplement 4):S304-S311. Available at: https://www.ncbi.nlm.nih.gov/pubmed/29043837.
- Alhazzani W, Moller MH, Arabi YM, et al. Surviving Sepsis Campaign: guidelines on the management of critically ill adults with Coronavirus Disease 2019 (COVID-19). Intensive Care Med. 2020;46(5):854-887. Available at: https://www.ncbi.nlm.nih.gov/pubmed/32222812.
- Gebistorf F, Karam O, Wetterslev J, Afshari A. Inhaled nitric oxide for acute respiratory distress syndrome (ARDS) in children and adults. Cochrane Database Syst Rev. 2016(6):CD002787. Available at: https://www.ncbi.nlm.nih.gov/pubmed/27347773.